The liquids cycle
Dive into the liquids cycle and learn how to ensure a safe and effective sterilization of liquid loads. Access this comprehensive article for detailed insights.

The sterilization of liquids in autoclaves is a common procedure in microbiology laboratories and research centers, where the sterility of liquids is essential for the integrity of scientific experiments and production processes.
Autoclaves, which operate using pressurized steam, are commonly employed to sterilize both instruments and solid objects. However, the sterilization of liquids, such as culture media and buffer solutions, presents unique challenges that influence the design and duration of the sterilization cycle to be used.
A critical aspect of liquid sterilization is the prevention of the boil-over effect, a phenomenon that occurs when a hot liquid in a sealed container undergoes a sudden change in pressure, causing spontaneous boiling and spillage. This risk, along with the need to carefully control the heating and cooling rates, distinguishes the sterilization of liquid loads from that of solid objects.
Fundamental principles of the liquids cycle in an autoclave
The liquids cycle in an autoclave operates on a modified gravity cycle, tailored to control the cooling phase and extend the duration of the heating phase. Although the sterilization temperature employed is 121°C, the duration depends significantly on the volume of the liquids and the size of the containers.
In contrast to gravity and vacuum cycles, which are designed for sterilizing solid and porous materials, the liquids cycle is specifically engineered for processing liquid loads in containers. This design aims to prevent sterilization failures, overheating of the load, spontaneous boiling, and to minimize evaporation loss.

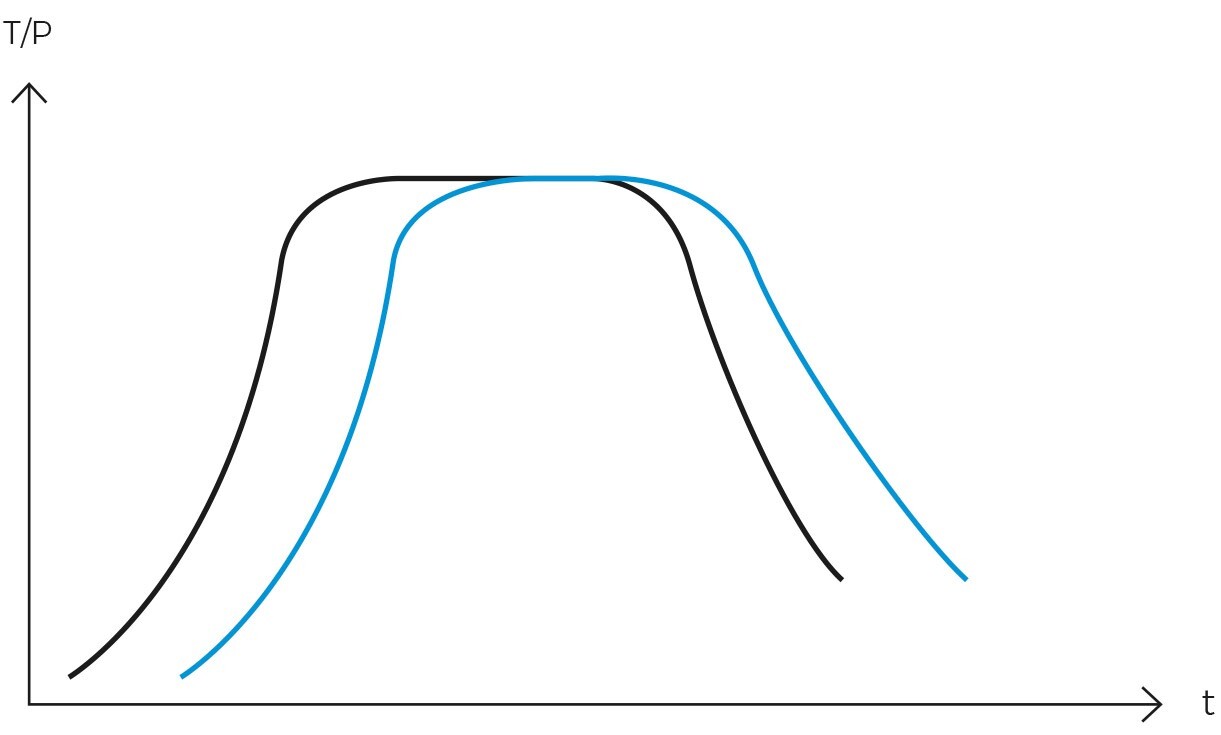
To achieve these objectives, precise control of the heating phase is crucial. Large volumes of liquids require extended heating times due to the significant delay in reaching equilibrium with the chamber temperature. Applying the same exposure time as a solid cycle for sterilizing a liquid load will result in the liquid not reaching the sterilization temperature as quickly.
The opposite effect occurs during the cooling phase, where liquids take significantly longer to cool. Inexperienced users risk burns when removing the load because, despite the chamber temperature having dropped to a safe level, the liquids may still be very hot.
Another important aspect to consider is that rapid depressurization during the cooling phase can cause a boil-over effect, or spontaneous boiling of the liquid. Therefore, the liquid cycle must depressurize the chamber gradually, slowly reducing the pressure to avoid abrupt changes.
Unique challenges in the sterilization of liquids
As previously discussed, the sterilization of liquids in autoclaves presents specific challenges due to the physical properties of liquids and the necessity to maintain their integrity throughout the process.
Handling the high specific heat of liquid loads
One of the primary challenges in liquid sterilization is their high specific heat. Compared to solids, liquids require significantly more energy to increase their temperature. This necessitates longer sterilization cycles for liquids, as additional time is needed during the heating phase for the liquid to reach the target sterilization temperature. Likewise, cooling also takes more time, extending the overall duration of the cycle.
To address this issue, modern autoclaves can be equipped with a central probe that monitors the internal temperature of the load and acts as a cycle regulator. This ensures that if a liquid cycle is programmed at a sterilization temperature of 119°C for 10 minutes, the timer does not start until the load temperature reaches 119°C.
In traditional autoclaves, the timer begins when the chamber temperature reaches 119°C, but the load temperature may only be 105°C. This discrepancy is a common cause of failures in correctly sterilizing liquid loads.
Preventing the boil-over effect
This phenomenon, also known as rapid boiling, is caused by a sudden pressure change during the cooling phase, which can result in splashing and spills, leading to the loss of sterilized load and, worse, contaminating the equipment and remaining load.
No one likes cleaning an autoclave with solidified agar residues on the chamber walls. To avoid this issue, a stepwise depressurization must be performed during the cooling phase, and precise temperature control of the load must be maintained using a central probe.
Maintaining the integrity of liquids
Another significant challenge is maintaining the chemical and biological integrity of liquids, especially since they take a long time to cool down, leading to overcooking and considerable time loss. This situation is particularly problematic for thermolabile liquids, whose properties can be adversely affected by unnecessary exposure to high temperatures. For example, certain culture media may exhibit reduced fertility rates due to the decomposition of proteins or triglycerides, while certain reagents may experience changes in their chemical composition.
To combat this issue and enhance laboratory productivity, it is recommended to use autoclaves with fast cooling systems, as they significantly reduce heat exposure time and allow faster load recovery, dramatically increasing laboratory productivity. Depending on the type of fast cooling system employed and the type of load, reductions in the duration of the cooling phase of up to 90% can be achieved, saving more than 60 minutes per sterilization cycle.
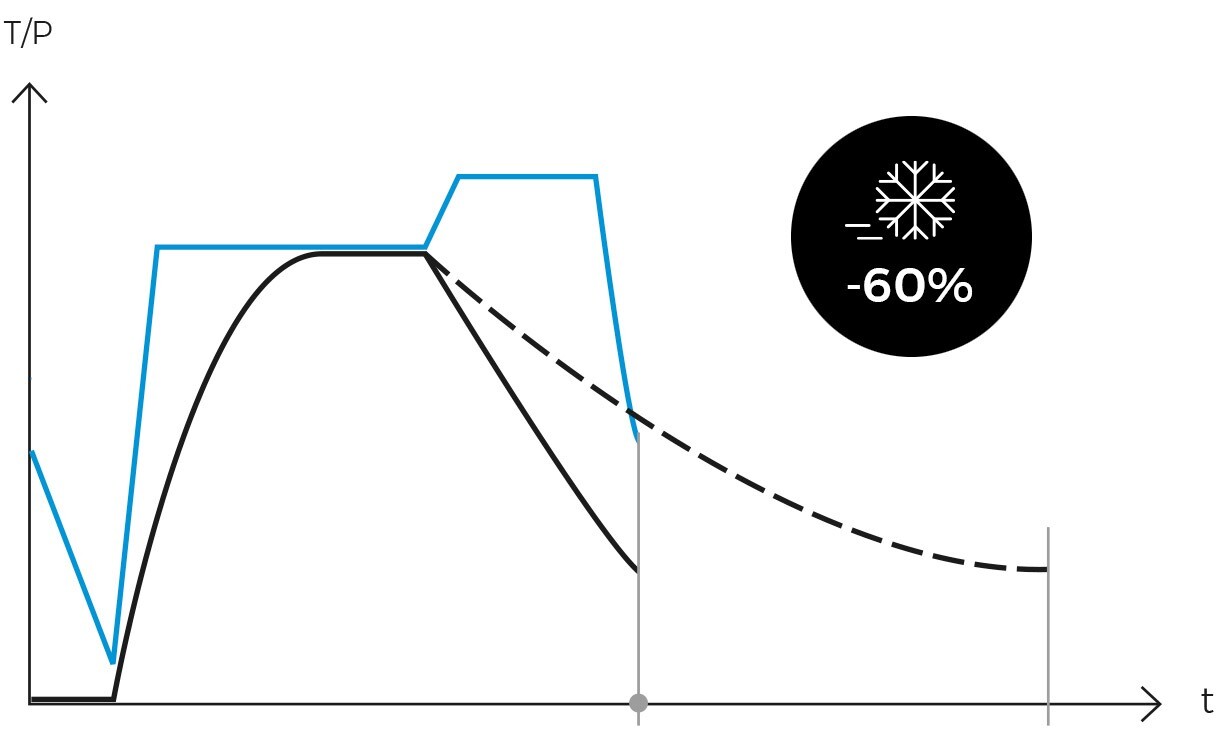
Among the most common technologies are fans and cooling coils. Additionally, modern autoclaves include pressure support systems to prevent boil-over during the cooling phase and minimize liquid loss through evaporation. It’s worth noting that even faster cycles can be achieved with antoher category of autoclaves, media preparators, which are purpose-built for processing large volumes of culture media.
Key parameters of the liquids cycle
As discussed, the liquids cycle in an autoclave is a delicate process requiring precise configuration of multiple parameters to ensure an effective and safe sterilization of liquid loads. These parameters include chamber temperature, load temperature, chamber pressure, exposure time, and control of pressure during the cooling phase, each of which plays an important role in the success of the process.
-
Optimal temperature and pressure
Temperature and pressure are the most critical factors in the sterilization of liquids. Generally, liquids are sterilized at a temperature of around 121°C, achieved under a pressure of approximately 1.1 Barg. This combination of high temperature and pressure is effective in eliminating microorganisms, including spores. However, for thermolabile liquids, lower temperatures are preferred.
It is essential to maintain these conditions consistently during the sterilization phase to ensure complete sterility of the liquid. Additionally, it is advisable to use a central probe to monitor the load temperature, which should govern the cycle instead of the chamber temperature.
-
Sterilization time
The exposure time at the sterilization temperature is another vital parameter. This time varies according to the type and volume of the liquid, as well as the total load in the autoclave. Liquids require a longer exposure time compared to solids due to their higher specific heat.
Typical exposure times can range from 15 minutes to more than 30 minutes, depending on these factors. Two recommendations to consider are using biological indicators to validate the processes and minimizing the volume of containers to reduce cycle times. It is more efficient to process more containers of smaller volume than fewer containers of larger volume.
Finally, it is recommended to employ F0-regulated sterilization cycles due to their ability to accurately quantify the lethality of a sterilization process. By using the F0 value, the sterilization cycle is automatically adjusted to the specific requirements of the load. This prevents inefficiencies from insufficient exposure times and consistency issues between different rotations related to different arrangements of the load within the autoclave, both in form and number of containers.
-
Control of the cooling phase
The cooling phase is an important stage in the liquids cycle. Rapid depressurization will cause uncontrolled boiling of the liquid load, while excessively slow cooling will unnecessarily prolong the cycle and ‘overcook’ the load, possibly degrading the quality of the processed liquid. Therefore, an autoclave equipped with liquids program should be used to avoid abrupt changes in temperature and pressure during the cooling phase.
For laboratories with demands for processing large volumes of liquids, it is recommended to employ autoclaves with fast cooling systems or media preparators to expedite this process. Such autoclaves can exponentially improve the productivity of the laboratory without compromising safety or efficacy.
-
Monitoring and validation
Monitoring and recording each process is essential to ensure that each sterilization cycle is performed correctly. This is generally achieved through sensors and automated controls that adjust temperature, pressure, and time as necessary. Furthermore, periodic validation of the autoclave’s performance is crucial to confirm its continued effectiveness over time.
Autoclaves and specific accessories for the sterilization of liquids
In the marketplace, numerous options are available to enhance the efficiency and safety of the sterilization of liquids, all of which leverage technologies and specialized models:
-
Autoclaves equipped with cycles for liquids
These autoclaves are equipped with control systems and specific programs for the sterilization of liquids. The most advanced models even allow programming by F₀ value instead of exposure time.
-
Autoclaves with a flexible probe
These provide real-time temperature readings of the conditions within the liquid load. This accessory ensures that sterilization is carried out correctly and that the load is exposed to the target temperature for the required duration.

-
Fast cooling systems
These systems shorten the cooling phase duration. Examples include the use of external fans, internal fans, a water cooling coil built around the chamber, a cooling jacket that surrounds the chamber, or water shower systems.
Special considerations for heat-sensitive liquid loads
The sterilization of thermolabile liquid loads necessitates a meticulous and tailored approach to ensure both the preservation of the physical and chemical integrity of the load and its sterility. These types of liquid loads, including certain chemical reagents and culture media, are susceptible to degradation or alteration of their properties when exposed to elevated temperatures for prolonged periods.
To mitigate this issue, it is advisable to utilize the thermal equivalence between different temperatures and exposure times through the use of the F₀ value.
Utilization of the F₀ value
The F₀ value allows for the quantification of the sterility of a thermal process and also the equivalence of lethality between different sterilization processes. This method is widely employed in the sterilization of pharmaceuticals and food products and is key for maintaining the integrity of substances prone to thermolysis.
Specifically, the F₀ value denotes the equivalent exposure duration, in minutes, at a reference temperature of 121°C. An F₀ of 3, for example, signifies a sterilization process comparable to three minutes at 121°C. To elucidate, let’s consider an empirical instance: applying the F₀ formula reveals that an F₀ of 3 corresponds to six minutes at 118°C. Consequently, three minutes at 121°C possesses the same microbial lethality as six minutes at 118°C, rendering both processes equally effective in terms of sterilization.
Fundamentally, the F₀ value enables the extrapolation of a process’s sterilizing effectiveness across different temperatures. This allows for the precise adjustment of a thermal process by altering its maximum temperature, thereby optimizing the balance between effective sterilization and the preservation of the product’s physicochemical properties.
Calculation the duration of a cycle governed by F₀
When utilizing an autoclave with F₀ programs, only the target F₀ value and the maximum process temperature need to be specified, eliminating the need to program a specific sterilization time. The autoclave automatically monitors the progression of the actual F₀ value and terminates the cycle upon reaching the target F₀ value.
Cooling of thermolabile liquids
A careful cooling phase is equally important for heat-sensitive liquids. Excessively slow cooling results in an excessive and unnecessary heat exposure, whereas rapid depressurization can cause splashing and spills. Therefore, it is highly recommended to use autoclaves equipped with a fast cooling system and pressure support to process such loads. This minimizes the time the load remains hot, ensuring optimal preservation of its properties.
Best practices and recommendations for an effective sterilization of liquids in autoclaves
To optimize the sterilization of liquids in an autoclave, we recommend adhering to the following practices:
-
Proper container selection
Always utilize heat-resistant containers and ensure adequate space is left for the thermal expansion of the liquids.
-
Always leave semi-open the containers with a cap
To prevent the rupture of containers or spills, liquids should never be sterilized in hermetically sealed containers unless a cycle with pressure support is employed. For instance, bottles with caps should be slightly loosened, and Erlenmeyer flasks should be covered with aluminum foil.
-
Correct autoclave parameter adjustment
Adjust the cycle duration according to the total volume of the containers being sterilized. It is essential to use an autoclave capable of performing a stepwise depressurization during the cooling phase.
-
Use autoclaves with liquid programs and a fast cooling system
This practice saves significant time, prevents overcooking of the load, enhances operator safety, and ultimately reduces cleaning time due to load spills or container breakage.

-
Monitoring and validation of the liquids cycle
Equip the autoclave with a flexible probe placed inside a reference container. This setup allows precise monitoring of the temperature evolution within the load and verifies that the load has been exposed to the target temperature for the necessary duration. It is also highly recommended to use biological and chemical indicators to confirm proper sterilization and to maintain detailed records of all executed processes.
-
Handling of the load
Avoid premature opening of the autoclave door and handle containers with care once the cycle is complete. Liquids require significantly more time to heat up than solid objects, and the same applies to the cooling phase.
-
Regular cleaning and maintenance of the autoclave
Maintain cleanliness of the autoclave and perform regular inspections and maintenance to ensure the proper functioning of safety mechanisms and to prolong the autoclave’s lifespan.
By following these practices, you can enhance the efficacy and safety of liquid sterilization in an autoclave, ensuring consistent and reliable results in any context.