Isothermal or low-temperature cycle
Explore how the isothermal or low-temperature cycle in autoclaves offers a solution for processing heat-sensitive materials. Read the article for more detailed information.

Sterilization is a critical process in various sectors, particularly in scientific research, where the complete eradication of all forms of life from an object is essential for the safety of researchers, the integrity of experimental results, and public health.
In this context, among the numerous available sterilization techniques, the isothermal cycle or low-temperature cycle using steam autoclaving stands out as an innovative and efficient solution for processing heat-sensitive objects or substances.
This process, conducted at a consistently low temperature, is ideal for disinfecting, pasteurizing and sterilizing instruments and materials that cannot withstand the high temperatures used in conventional sterilization cycles. In fact, low-temperature sterilization is often the only viable option for processing thermolabile loads, such as certain plastics, electronic devices, and biological solutions.

The principle behind isothermal sterilization is to maintain the temperature at a level that is sufficiently high to destroy any microorganisms, yet low enough to avoid causing irreversible damage to the materials being processed.
This balance is achieved through the use of carefully designed programs that maintain a constant temperature throughout the process. These programs are typically either of long duration or repetitive. This technique ensures that heat is uniformly and effectively distributed across all surfaces of the load, thereby destroying any form of life without compromising the structural integrity of the instruments or materials processed.
A significant advantage of this method is its ability to sterilize without altering the physical or chemical properties of the treated objects. This is particularly important for complex electronic devices, such as certain implants, which may have components that are thermolabile or sensitive to excessive moisture.
In the research and development of pharmaceutical and biotechnological products, preserving the physicochemical properties of proteins is crucial. For instance, in the preparation of specific culture media, the low-temperature isothermal cycle allows these products to be sterilized without overheating, thus preventing degradation or alteration of their formula, and preserving their fertility rates.
Principles of isothermal processing
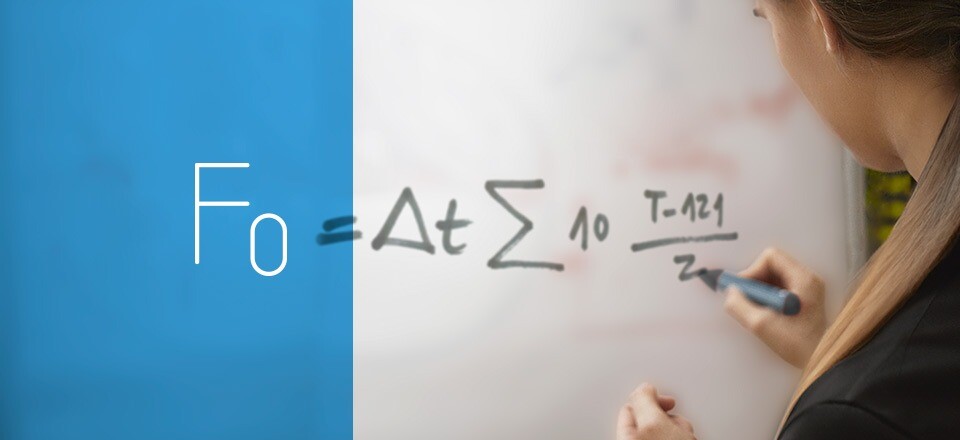
Isothermal processing, an advanced technique in the field of sterilization, is grounded in specific thermodynamic principles to achieve effective pasteurization or sterilization of heat-sensitive materials. This method is distinguished by its approach of maintaining a constant temperature throughout the process, allowing for safe and effective pasteurization or sterilization without compromising the integrity of the treated objects.
Thermodynamic foundations
The isothermal process is characterized by its ability to maintain a constant system temperature. In the context of autoclave sterilization, this implies that heat transfer to or from the system is managed in a manner that preserves thermal equilibrium. This equilibrium is crucial for preventing temperature fluctuations that could damage sensitive materials or cause insufficient lethality in certain regions of the load.
Isothermal sterilization leverages this principle to ensure that the temperature remains within a specific range, sufficient to destroy microorganisms without reaching the thermal damage point of the structure or composition of the sterilized objects.
Differentiation from other sterilization methods
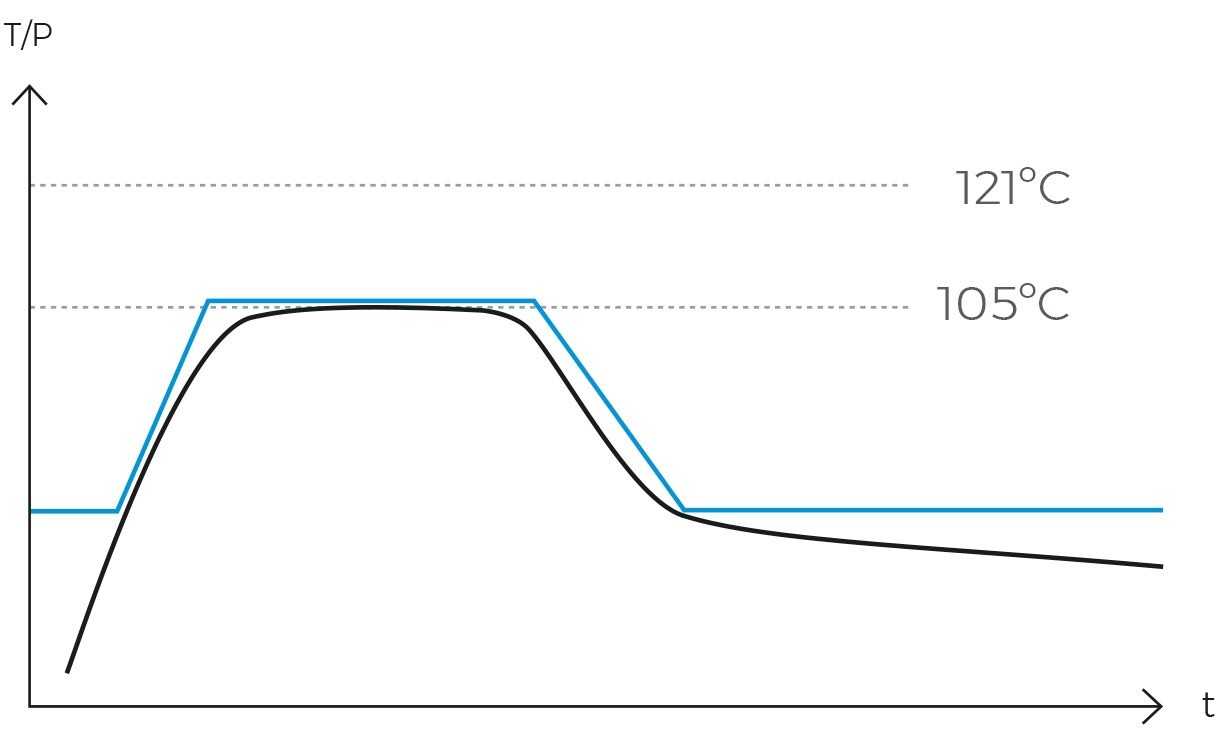
Unlike conventional sterilization methods, such as high-temperature steam sterilization, the low-temperature cycle does not rely on brief exposures to very high temperatures to achieve sterilization. Instead, it focuses on a less aggressive approach, utilizing prolonged exposures at lower temperatures.
While traditional methods typically operate at temperatures exceeding 120°C, isothermal sterilization operates at a much lower temperature range, making it ideal for materials that cannot withstand extreme heat.
Mechanism of action
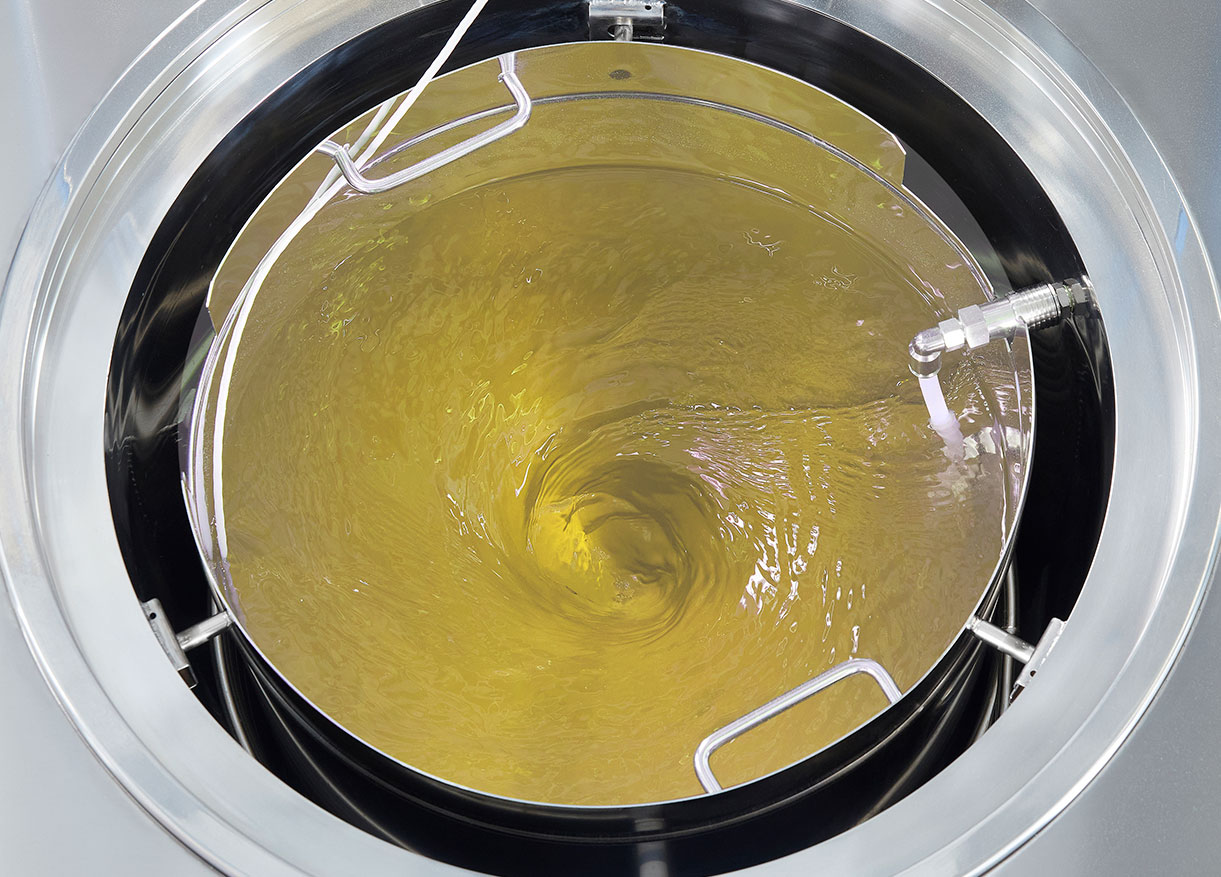
The mechanism of action in isothermal steam autoclave sterilization involves the use of controlled temperature moist heat to destroy microorganisms. Moist heat is effective at denaturing the proteins within the cell walls of microorganisms, leading to their death or inactivation.
By operating at lower temperatures, this method reduces the risk of damaging heat-sensitive materials, such as certain plastics, electronic devices, and biological preparations.
Applications of the isothermal Cycle
The isothermal sterilization cycle, characterized by its ability to operate at controlled and constant temperatures, has a broad spectrum of applications, particularly in environments where the integrity of heat-sensitive materials is of paramount concern.
This method has become an indispensable tool across various fields, ranging from scientific research to the production of pharmaceuticals.
-
Use in microbiology laboratories for the preparation of culture media
In the realm of microbiology laboratories, the isothermal cycle is often used for the preparation of culture media and agar. These materials are crucial for the cultivation of microorganisms in microbiological and biotechnological studies. Isothermal sterilization ensures that these media are sterilized without altering their chemical composition.
-
Sterilization of sensitive materials in research
The isothermal cycle is also employed for the sterilization of a variety of sensitive materials used in research. This includes certain types of plastics, chemical reagents, and biological components that could degrade or lose their efficacy under more aggressive sterilization conditions.
The ability to precisely control the temperature allows these materials to be sterilized safely, preserving their integrity and properties.
-
Sterilization of thermolabile medical devices
One of the most critical applications of the low-temperature cycle is in the sterilization of medical devices. Many of these devices contain components that are sensitive to high temperatures, such as certain plastics, adhesives, or integrated electronic components.
Isothermal sterilization enables effective sterilization of these devices without compromising their functionality or structural integrity. This is particularly relevant for advanced surgical instruments, implants, and diagnostic devices that require a high degree of precision and reliability to operate effectively.
Configuration and temperature range in isothermal sterilization
The configuration and temperature range are critical aspects of the isothermal sterilization cycle, determining its efficacy and applicability in various contexts. The flexibility in temperature configuration allows the isothermal cycle to adapt to a variety of specific needs, ensuring the effective sterilization of heat-sensitive materials without compromising their integrity.
Operating temperature range
The low-temperature cycle typically operates within a temperature range of 70°C to 95°C. This range is significantly lower than the temperatures used in conventional sterilization methods, such as high-pressure steam cycles, which commonly reach 121°C or higher.
The ability to operate at these lower temperatures is what makes the isothermal cycle ideal for materials that cannot withstand extreme heat.
Temperature settings and flexibility
One of the most notable advantages of the isothermal cycle is its ability to adjust the temperature according to the specific needs of the material being sterilized.
This flexibility allows users to select the optimal temperature that ensures the effective elimination of microorganisms while minimizing the risk of thermal damage to sensitive materials.
This adjustment capability is highly advantageous in applications where different materials require different levels of thermal exposure.

Precise temperature control
Precise temperature control is fundamental in the isothermal cycle. Autoclaves equipped for isothermal cycles are designed with advanced temperature control systems that maintain the desired temperature with minimal variation.
This precise control is essential to ensure that the entire sterilization process is carried out uniformly and effectively, avoiding cold spots that could lead to incomplete sterilization and hot spots that could damage the structural integrity of the load.
Advantages and limitations of the isothermal sterilization cycle
The isothermal sterilization cycle, characterized by its use of controlled and constant temperatures, presents several significant advantages, particularly in the treatment of heat-sensitive materials. However, like any method, it also has certain limitations that must be considered.
Advantages of the low-temperature or isothermal cycle
-
Protection of heat-sensitive materials
The primary advantage of the isothermal cycle is its ability to sterilize materials that cannot withstand the high temperatures of conventional methods. This includes certain plastics, electronic devices, and biological materials, whose integrity remains largely intact after processing.
-
Precise temperature control
The isothermal cycle allows for precise control of temperature, which is crucial for ensuring effective sterilization without exceeding the thermal damage threshold of the materials.
-
Efficacy in microorganism elimination
Despite operating at lower temperatures, the isothermal cycle is effective in eliminating a large part or the totality of microorganisms, including bacteria and viruses, by operating over much longer time periods. This ensures safety and sterility.
-
Versatility in various applications
Its ability to be adjusted to different temperature ranges makes it suitable for a wide range of applications, from the sterilization of medical devices to the preparation of specific culture media in microbiology laboratories.
Limitations of the low-temperature or isothermal cycle
-
Longer cycle time
Due to the lower temperatures used, isothermal cycles often require significantly more time to achieve effective sterility compared to high-temperature methods. This could be a limiting factor in environments with high turnover and where productivity is a critical metric.
-
Restrictions on types of materials
While ideal for heat-sensitive materials, the isothermal cycle is not suitable for all types of items. Some objects may require the higher temperatures of traditional methods to ensure adequate sterilization, especially those heavily contaminated or containing prions or spores.
-
Cost and equipment availability
Autoclaves capable of performing isothermal cycles tend to be more expensive and less common than standard autoclaves, which could limit their accessibility in economically constrained settings.
-
Specific safety and maintenance considerations
The operation and maintenance of these autoclaves are comparable to standard autoclaves, requiring specific knowledge and, in some cases, additional precautions. This is particularly true regarding periodic checks to certify the proper functioning of the equipment.
Standard operating procedures and protocols in isothermal sterilization
The correct implementation of an isothermal sterilization protocol necessitates thorough preparation and validation testing. These steps are critical to ensure the efficacy of the sterilization process, preserving the safety and integrity of the treated materials.
-
Preparation of materials
Prior to sterilization, all materials must be meticulously cleaned and disinfected. High microbial load on items to be sterilized hinders effective sterilization. Organic or inorganic residues can interfere with the sterilization efficacy. Materials should be arranged to allow free air circulation.
-
Loading the autoclave
Materials must be placed in the autoclave in a manner that allows uniform heat distribution. If baskets are stacked, the bottom of the upper basket should not touch the materials in the lower basket. Avoiding chamber overloading is crucial to ensure effective sterilization.
It is recommended to select the combination of temperature and time based on the material type and the manufacturer’s specifications of the object to be processed.
-
Sterilization process
Once the autoclave is loaded and the cycle selected, the autoclave program is initiated. The equipment will heat up, raising the internal chamber temperature to the set value for the isothermal cycle.
During the cycle, the temperature remains constant at the set value or within the selected range. Temperature stability is essential for process efficacy. Modern isothermal autoclaves are equipped with controls to monitor and adjust temperature and pressure, ensuring the cycle stays within the established parameters.
-
Cycle completion and post-process
Upon cycle completion, materials must be cooled in a controlled manner to prevent condensation and damage from abrupt temperature changes. Once cooled, materials can be removed from the autoclave.
It is important to handle them with care to maintain sterility. Sterilized materials should be stored in a clean, dry environment to avoid recontamination.
-
Safety and maintenance considerations
Operators must be adequately trained in the use of the autoclave and adhere to all safety measures, including the use of personal protective equipment.
Additionally, autoclaves should undergo regular maintenance to ensure optimal performance and safety.